Stevens Researcher Has Skin, Heart, and Soul in the Game of Solving Biomedical Challenges
For Stevens Institute of Technology electrical and computer engineering assistant professor Negar Tavassolian, developing algorithms and learning-based systems to support biomedical devices with life-saving potential is more than abstract research.
"I've always been interested in solving medical problems with commercially viable technology," Tavassolian says. "I like to make things and see how they can help people."
Her work, which is affiliated with the Stevens Institute for Artificial Intelligence, is showing promise that can help many people, especially those who may not know they have serious medical conditions ranging from skin cancer to heart failure.
When skin-deep really is good enough
Tavassolian was granted a National Science Foundation (NSF) CAREER award to develop an innovative, portable dermatological application that will create a high-resolution image of a patient's skin for early detection of skin cancers. To do that, she leverages millimeter-wave technology with artificial intelligence and other emerging technologies.
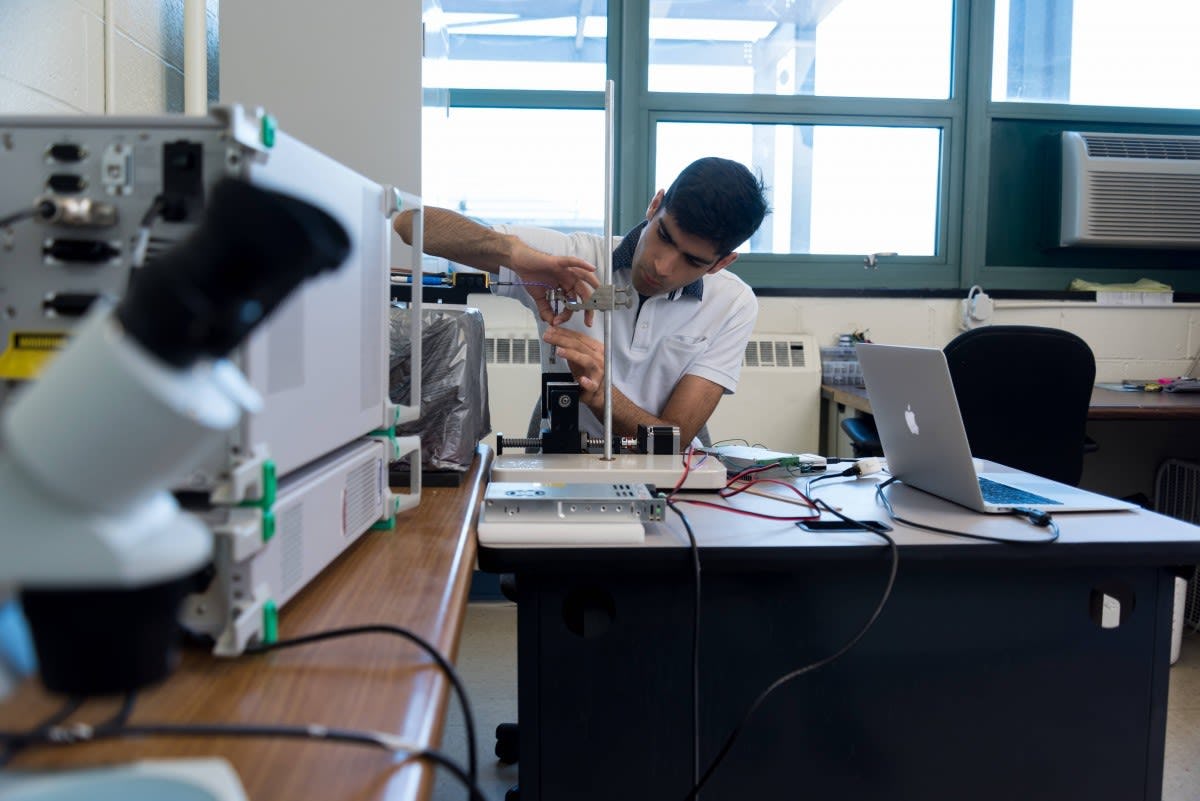
Millimeter-wave imaging (at a frequency of 30 to 300 gigahertz) is cheaper, safer, less power-intensive and much more portable than other types of body imaging that exist today. The technology doesn’t go deep enough to penetrate internal organs, but it's ideally suited for superficial imaging. Tavassolian and graduate assistant Amir Mirbeik are splitting those millimeter-wave bandwidths into smaller channels, then processing and reassembling the slices to create detailed images for medical diagnoses.
"Our goal is to have a device that the doctor holds over the tissue to see whether a lesion is a malignant cancer or not," she explains. "Our technology provides in-depth visualization that can go up to two and a half millimeters deeper into the skin to see a 3D profile of any tumor. Healthy skin has lower water content than a tumor, and the millimeter-wave-created image can detect that difference with higher contrast than is currently possible. A lot of times, there's discoloration with a tumor, but around the discoloration, there are more cancer cells that are the same color as the skin. You won't see that with your eyes—but we can see it with this technology."
It's intended to be a complement to, rather than a replacement for, current cancer detection methods.
"It's not meant to replace biopsies, which are the gold standard," she says. "Rather, it's meant to ensure consistent, accurate care by both reducing unnecessary biopsies and finding tumors earlier."
Tavassolian's research isn't the first in this space, but she's working to ensure it's the best.
"There are other handheld technologies," she notes, "but they have very high false positives. They're also quite expensive, as much as $50,000 each. Our goal is to make a device for $1,000, so every dermatologist can have one."
Wearing your heart on your monitor
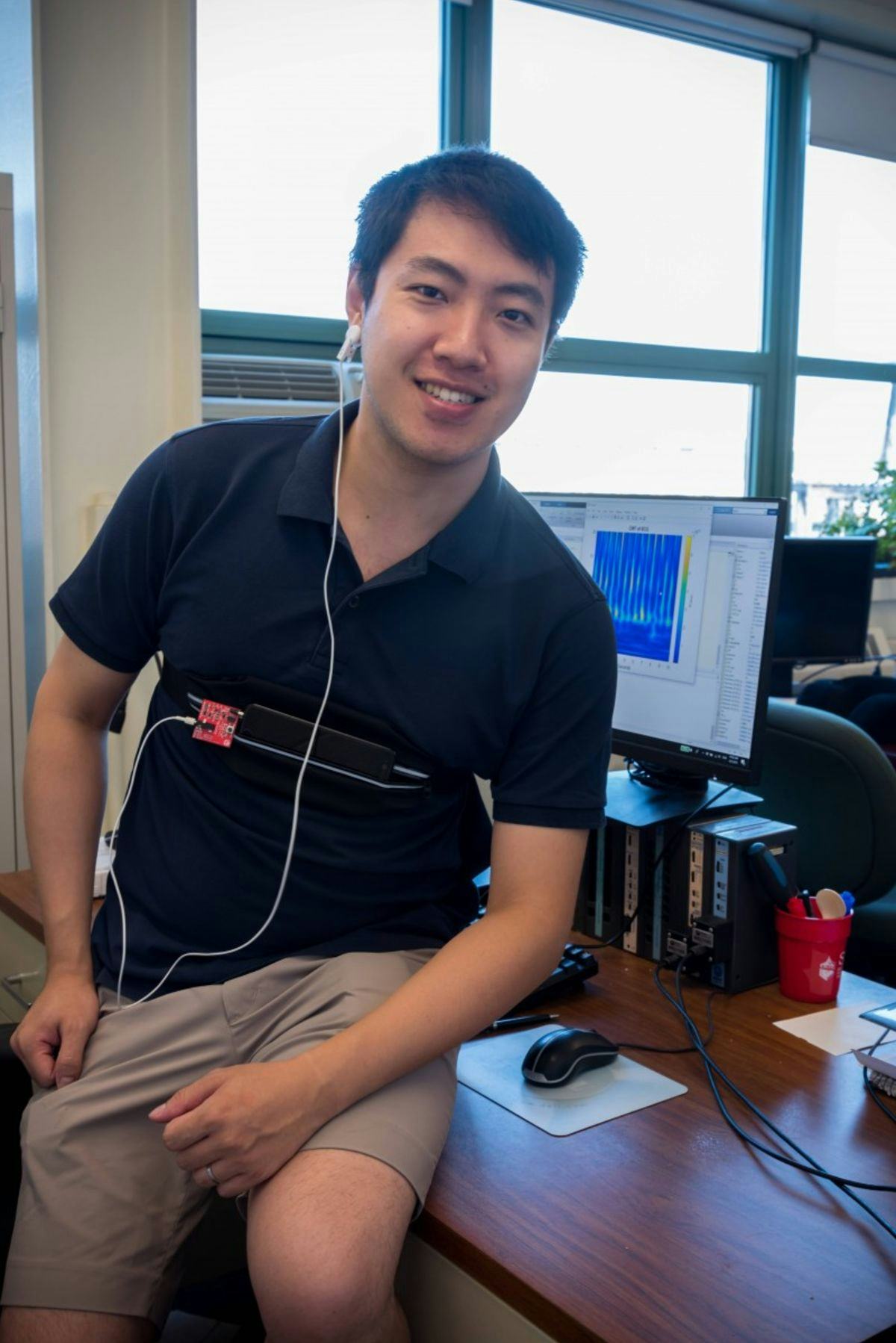
Tavassolian is also hunting for heartbeat irregularities by using tiny yet powerful motion sensors, strapped over people's chests or placed like an earbud in their ears.
These sensors collect huge quantities of data, which are in turn run through intelligent digital signal processing techniques that reduce or even cancel the impact of motions such as walking and breathing from the heartbeat signals. Machine-learning-driven algorithms differentiate the signals of healthy patients from those who may be at risk for heart attack, heart failure or hypertensive heart disease. Her doctoral student, Chenxi Yang, has presented seven papers on this technology—including one at the IEEE Engineering in Medicine and Biology conference this past August—and currently has two journal papers under review.
"The device has a gyroscope and accelerometer that pick up vibrations to deliver data about linear and rotational motions of the chest wall," Tavassolian explains, "providing highly accurate heartbeat measurements that can provide an early, real-time warning for potential cardiovascular issues."
And it happens more quickly, less expensively and more comfortably than other methods allow. Early testing with Columbia University Medical Center has demonstrated accurate classification up to 99.5 percent.
"We have even tracked 'pulse transit time,' the time difference between the cardio-mechanicals signals and an optical sensor, to monitor blood pressure in real time without the traditional cuff device," adds Tavassolian.
Touchless heart monitoring is also on the radar
And if you don't want to–or can't–sport even a miniscule heart monitor, Tavassolian has a solution for you too.
"Athletes, emergency responders and airplane pilots are just some of the people who could benefit from real-time monitoring of their vital signs, but can't risk hindering their motion with a wearable device," Tavassolian notes. "Babies don’t want anything attached to them, and seniors sometimes forget to put theirs on. But if we could find heartbeat abnormalities in these often high-risk populations in real time, we could save lives."
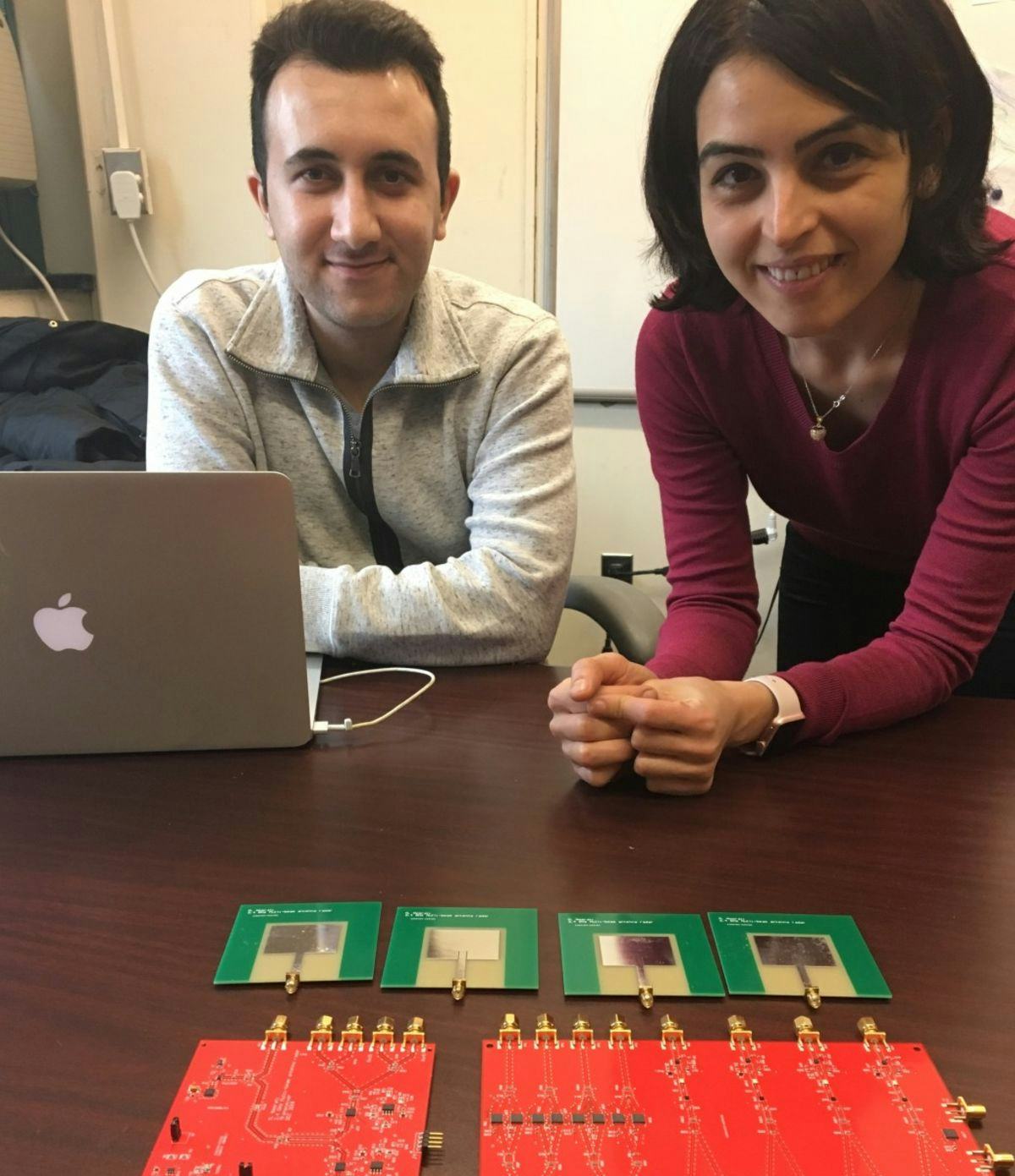
Tavassolian and doctoral student Mehrdad Nosrati are striving to do just that, developing technology to use low-cost, innovative Doppler radars to sense and measure heartbeats and respiration rates even in noisy, crowded settings, without ever touching the individual being monitored.
"We're using the same multiple-input and multiple-output, or MIMO, signal processing that's used in cell phones, but it has never been used before in radar," Tavassolian says. "We're borrowing that approach to increase the capacity of radar detection, and we've already deployed the system to reach acceptable accuracy at roughly 4½ feet. So far, we're focusing on biomedical applications such as multiple heartbeats, but we see many other applications, such as measuring velocity and scanning multiple lanes and vehicles at a toll gate."
Impressive as these applications are, Tavassolian doesn’t think of them as successful until they become commercially available. "I design everything with commercialization in mind," she says.
"I like to see results."