Stevens Heart-Monitoring Systems Integrate Wearable Sensors, Radars and AI to Listen To Your Heartbeat
Collaborations with Columbia University Medical Center, Rutgers could lead to better, cheaper detection of heart failure, heart attack and other cardiovascular issues
Monitoring the heartbeats and vital signs of athletes, emergency responders and hospitalized patients in real time, without hindering their motion, has long been a tough medical challenge to crack. With more than 2,000 deaths from cardiovascular disease each day in the U.S. alone, that challenge has never been more urgent.
A Stevens Institute of Technology researcher is testing two novel ideas that may help solve the puzzle.
"Heart failure (HF), for example, is a serious problem that afflicts 5 million to 6 million Americans, and the number is expected to rise," notes Stevens electrical and computer engineering professor Negar Tavassolian. "Yet the current heart-monitoring technology, the Holter system, is bulky, uncomfortable and expensive.
"By using both wearable, miniaturized cardio-mechanical sensors and novel radar architectures, we believe we can improve this monitoring."
Calibrating chest motions to calculate heartbeats
In one project, Tavassolian and doctoral student Chenxi Yang harvest data from small, lightweight motion sensors strapped to the chest with Velcro.
The monitors, about the shape and size of a single domino, are far smaller and lighter than the current Holter technology. Tiny gyroscopes and accelerometers within the devices collect and transmit data about linear and rotational motions of the chest wall that can be processed to extract highly accurate heartbeat measurements — and to warn of irregularities such as HF or hypertensive heart disease.
"One big advantage of this system is that these sensors do not need to be attached directly to the skin, and can instead be worn over clothing," notes Tavassolian. "We also hear from the patients that this system is more comfortable."
To detect potential abnormalities, Tavassolian and Yang will use intelligent digital signal processing techniques to process the vast quantities of data collected by the tiny, yet powerful, sensors. Algorithms will separate out human motions such as walking and breathing from the heartbeat signals; then additional machine-learning-driven classification algorithms will compare signals from cardiac disease patients with normal heartbeat data gleaned from healthy subjects.
In early testing with an experimental set of subjects wearing the monitors — 13 cardiovascular patients tested in collaboration with Dr. Philip Green at the Center for Interventional Cardiology at Columbia University Medical Center, and 30 healthy subjects on the Stevens campus — Tavassolian and Yang collected data demonstrating enhanced classification of normal and abnormal heartbeats, with accuracies from 98 to 99.5 percent.
"This wearable system could be used to warn patients to go to the physician," explains Yang. "It is not a spot diagnosis, but rather a warning that something is not right and a doctor should be seen right away."
An additional advantage of the system, notes Tavassolian, is that it will theoretically collect more accurate real-time data from subjects who are constantly moving, such as athletes and firefighters. Algorithms in development will smoothen and factor out the noise produced by constant motions.
Building onto the system, Tavassolian has also pilot-tested an unobtrusive earpiece to add blood-pressure measurements to the data-stream mix. Developed in collaboration with adjunct Stevens professor Yingying Chen and Rutgers University, the component works via a simple smartphone app.
"By calculating a metric called 'pulse transit time,' measured by the time difference between the cardio-mechanicals signals and an optical sensor," explains Tavassolian, "we have also monitored blood pressure in real time without the need for an uncomfortable cuff-based device."
Radar readings as heart monitors
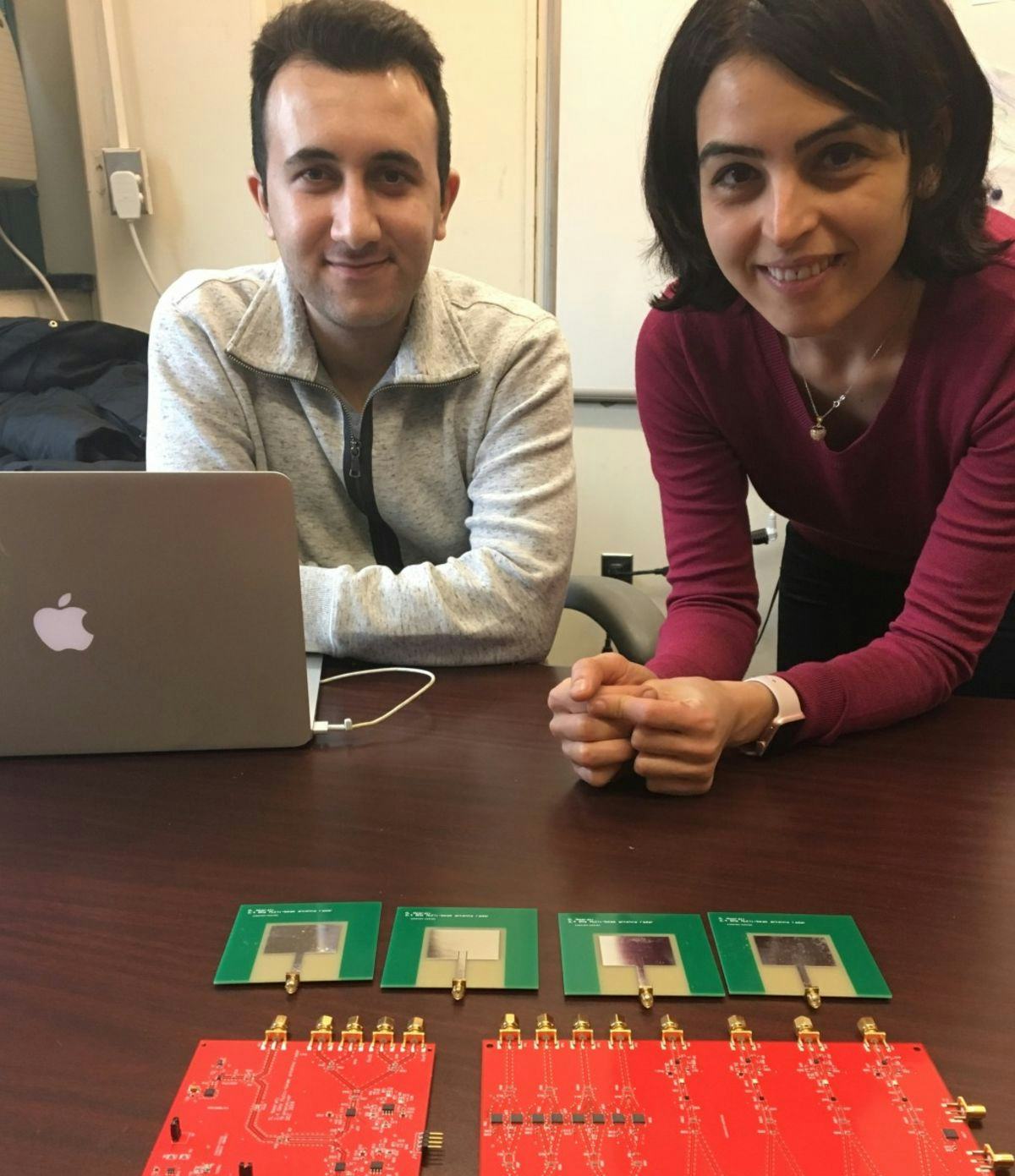
Tavassolian's second monitoring project, with doctoral student Mehrdad Nosrati, proposes the use of low-cost, innovative Doppler radars to sense and measure heartbeats and respiration rates without any contact with the bodies of individual or groups of people in a room.
The technology could prove useful in hospital environments: a room with the technology embedded, for example, might touchlessly scan patients for vital signs while also factoring in (and discarding) the extraneous vital signs of doctors, nurses and orderlies passing through the room.
Initial tests on a small set of subjects demonstrated that the concept is feasible. Heartbeat intervals calculated using an optimized antenna configurations broadcast at the frequency of 2.4 Gigahertz (the same frequency used by current WiFi technology) and enhanced signal processing methods matched real-time fingertip pulse readings of the same subjects more than 98 percent of the time.
"For now, we can only deploy the system as far as about 4½ feet away to reach an acceptable accuracy," explains Nosrati, who was awarded a $7,000 fellowship from IEEE's Medical Applications Fellowship Program to continue pursuing the research. "In the future, we will be working to increase the range."
Using beam-forming arrays of antennae, the duo soon hopes to bring the technology from the laboratory to medical settings, detecting the vital signs of multiple subjects in a space simultaneously. Arrays of the small, specially fabricated antennae will create two focused scanning beams that can detect multiple subjects' heartbeats with significantly enhanced accuracy and detection range.
"There are also many other potential applications of this technology, as well," concludes Tavasollian. "Imagine scanning multiple lanes and vehicles at a toll gate using a single device, or monitoring patients' heartbeats in a hospital with a single scanner placed in the ceiling. Once we have developed the technology further, we will see where else it may take us."