Stevens Students Make a Common Medical Procedure Safer for the Littlest Patients
Student team’s device alerts caregivers to respiratory distress in pediatric tracheostomy patients
If you’ve ever watched an episode of Grey’s Anatomy, House, or ER, you’ve likely seen someone perform a tracheostomy—a procedure to create an opening in the windpipe to help a patient breathe. While it makes for great television, these critical procedures are fairly common with more than 100,000 performed annually according to the National Institutes of Health.
Common as the procedures are, they are still risky: "48 percent of patients will experience a complication with a tracheostomy tube—an obstruction or something that disrupts their flow of oxygen," says Julianna Ricci, a senior at Stevens Institute of Technology. "That puts a lot of people at risk across the board." Adult patients can express their distress, but pediatric patients—especially the youngest children—lack the communication skills to signal when something’s wrong. And for pediatric patients, a blockage in the tube is the most common tracheostomy-related cause of death.
Ricci and four fellow biomedical engineering students—Franzisca Komar, Matthew Iobst, Kenneth Poser, and Yanique Spigner—teamed up as part of their senior design project to create a device to monitor the pediatric tracheostomy patients and alert caregivers of respiratory distress.
"It’s a way to help. That’s what biomedical engineering is—a way to help," says Komar.
Monitoring the littlest patients
When the team first took on the project, they envisioned redesigning the tracheostomy tube itself. But an eye-opening visit to an intensive care unit changed their minds. The team observed two young tracheostomy patients and watched as nurses monitored and cared for them.
"Seeing it in real life and hearing them suction [the tubes of] patients, it was very intense," says Spigner. The students realized there’s often a lag time between when a child first experiences a problem with their tracheostomy tube and when the medical staff recognizes it. "We all thought the procedure needed to be revamped and this was something we could help," says Spigner.
Meeting the patients made a big impact. The young patients, roughly two years old, were active, lively, and playful and they wanted to get up and move around. Yet, they were confined to healthcare facilities and connected to cumbersome monitors for around-the-clock observation. "The current technology in use requires patients to be stationary. It’s not portable—or kid friendly," says Poser.
The visit motivated the Stevens students to find a solution specifically designed for pediatric patients, primarily under the age of two, and helped them envision their device—TrachAlert. "Our end goal is anything that will allow patients to be more mobile, even if parents are able to come in and play more with the patients," says Poser. "It’s more peace of mind among patients, parents, and caregivers. That way, everyone can monitor the kids."
TrachAlert
After nailing down a plan of action, the team quickly zeroed in on the design and specifications of their device. The students wanted to create something that would be small and portable, allowing the children to be more active and autonomous. It’s a problem that their clinical advisor, Dr. Frank Castello, clinical associate professor of pediatrics at Rutgers-Robert Wood Johnson Medical School, has wanted to solve for years.
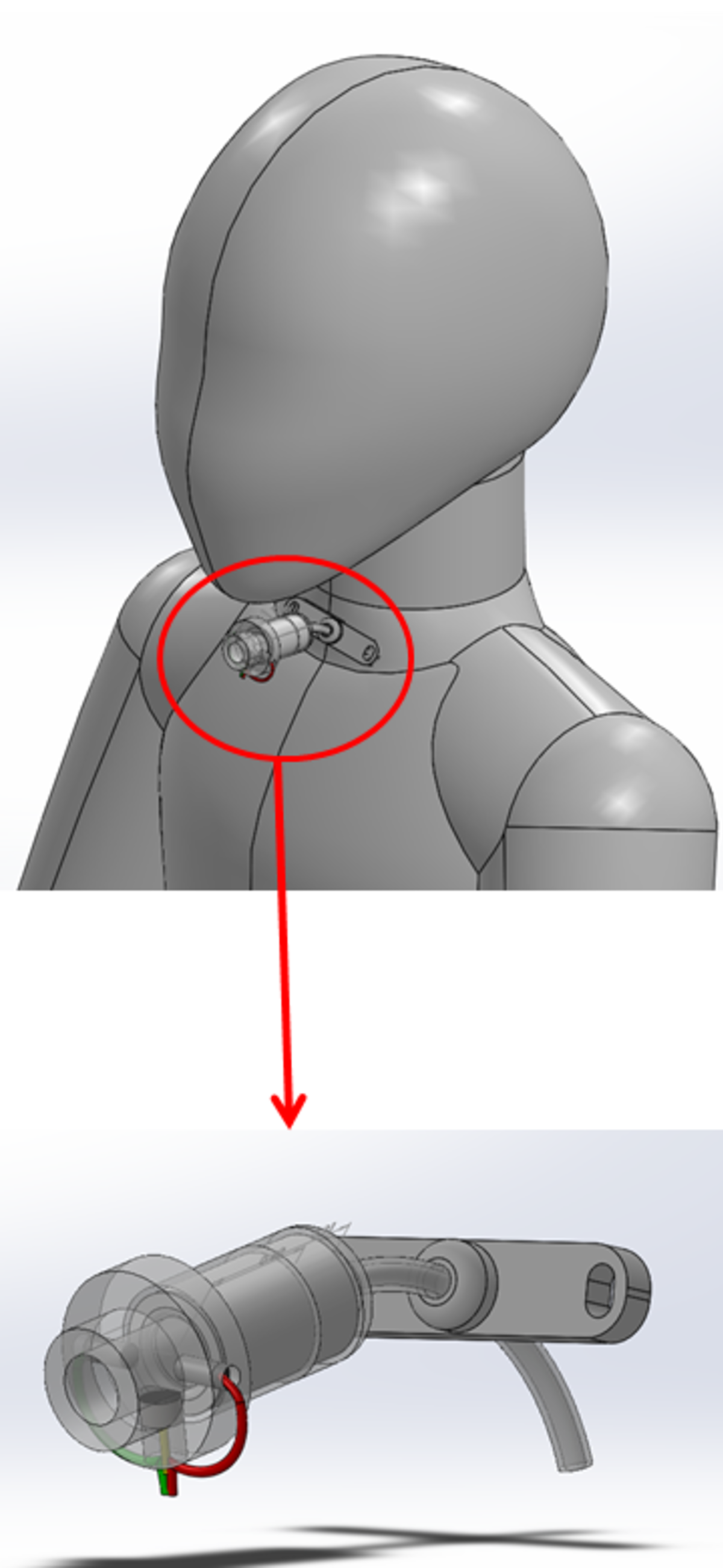
Since pediatric tracheostomy tubes are only 15 millimeters in diameter, the team had to consider several constraints when designing TrachAlert. "There are other devices on the market for tracheostomy tubes to support breathing functions. We looked at similar devices and asked how can we make it small enough so it’s not going to impact the components of the tube itself while effectively monitoring it," says Iobst, who came up with the TrachAlert’s design. It also needs to be easily removed in case a caregiver must adjust or suction secretions from the tube.
TrachAlert will use a sensor to detect breathing patterns and identify if and when there’s an obstruction in the airway. "We’re simulating a blockage and analyzing the data to determine whether or not the device effectively detects an obstruction," says Komar.
Creating a working prototype
Figuring out the electrical components was the biggest challenge. Since no one on the team is an electrical engineer, they had to hit the ground running and learn on the fly. Spigner devoted herself to this aspect of the project, investing lots of time and effort on top of her classes and the rest of the project to become the team’s anchor for all things electric.
The team also studied invention disclosure, the patent process, and FDA checkpoints, too.
The students didn’t expect their project to be as far along as it is now. They’ve created a working prototype, including the housing, electrical components, sensor, and preliminary codes, and are currently testing the device. They’ve presented their work several times this spring, including at the Northeast Bioengineering Conference and to the Stevens Institute of Technology patent committee, and will share their prototype work at Stevens’ Innovation Expo on May 3.
"Going from an idea to an actual product is not something many college seniors can say they’ve done," says Komar.
Ultimately, the team hopes to patent and license the design so the device can be manufactured. They think TrachAlert can make a real difference in the lives of tracheostomy patients who may experience communication barriers.
See this project and many others at the 2019 Stevens Innovation Expo on May 3.